The price of greatness is responsibility
If you have a hard problem , try the best to cleared well immediately
If you want something that you can't get it , try the best of everything that you can do it . If you needed other's , said to other to help you .
If you have a hard problem , try the best to cleared well immediately
If you want something that you can't get it , try the best of everything that you can do it . If you needed other's , said to other to help you .
| Thiamine | |
|---|---|
 | |
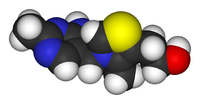 | |
| IUPAC name | 2-[3-[(4-amino- 2-methyl- pyrimidin- 5-yl) methyl]- 4-methyl- thiazol- 5-yl] ethanol |
| Other names | Aneurine hydrochloride, thiamin |
| Identifiers | |
| CAS number | 59-43-8 (Cl-) |
| PubChem | 1130 |
| MeSH | Thiamine |
| SMILES | [Cl-].Cc1c(CCO)sc[n+]1Cc2cncnc2N |
| ChemSpider ID | 5819 |
| Properties | |
| Molecular formula | C12H17N4OS+Cl-.HCl |
| Molar mass | 337.27 |
| Melting point | 248-260 °C (hydrochloride salt) |
| Hazards | |
| Main hazards | Allergies |
Chemical properties
Thiamine is a colorless compound with a chemical formula C12H17N4OS. Its structure contains a pyrimidinethiazole ring linked by a methylene bridge. Thiamine is soluble in water, methanol, and glycerol and practically insoluble in acetone, ether, chloroform, and benzene. It is stable at acidic pH, but is unstable in alkaline solutions. Thiamine is unstable to heat, but stable during frozen storage. It is unstable when exposed to ultraviolet light and gamma irradiation. Thiamine reacts strongly in Maillard-type reactions. ring and a
Biosynthesis
Complex thiamine biosynthetic pathways occur in bacteria, some protozoans, plants and fungi. The thiazolepyrimidine moieties are synthesized separately and then assembled to form ThMP by thiamine-phosphate synthase (EC 2.5.1.3). The exact biosynthetic pathways may differ among organisms. In E. coli and other enterobacteriaceae ThMP may be phosphorylated to the cofactor ThDP by a thiamine-phosphate kinase (ThMP + ATP → ThDP + ADP, EC 2.7.4.16). In most bacteria and in eukaryotes, ThMP is hydrolyzed to thiamine, that may then be pyrophosphorylated to ThDP by thiamine diphosphokinase (thiamine + ATP → ThDP + AMP, EC 2.7.6.2). and
The biosynthetic pathways are regulated by riboswitches in all organisms that synthesise thiamine. If there is sufficient thiamine present in the cell then the thiamine binds to the mRNA encoding genes required in the pathway preventing the translation of the enzymes. If there is no thiamine present then there is no inhibition and the enzymes required for the biosynthesis are produced. The specific riboswitch, the TPP riboswitch, is the only riboswitch that has been identified in both eukaryotic and prokaryotic organisms.
Nutrition
References
Thiamine is found in a wide variety of foods at low concentrations. Yeast and pork are the most highly concentrated sources of thiamine. Cereal grains, however, are generally the most important dietary sources of thiamine, by virtue of their ubiquity. Of these, whole grains contain more thiamine than refined grains, as thiamine is found mostly in the outer layers of the grain and in the germ (which are removed during the refining process). For example, 100 g of whole wheat flour contains 0.55 mg of thiamine, while 100 g of white flour only contains 0.06 mg of thiamine. In the US, processed flour must be enriched with thiamine mononitrate (along with niacin, ferrous iron, riboflavin and folic acid) to replace that lost in processing.
Some other foods rich in thiamine are oatmeal, flax and Sunflower seeds, brown rice, whole grain rye, asparagus, kale, cauliflower, potatoes, oranges, liver (beef, pork and chicken) and eggs.
Thiamine hydrochloride is a food additive used to add a brothy/meaty flavor to gravies or soups.
Reference Daily Intake and high doses
The RDA in most countries is set at about 1.4 mg. However, tests on volunteers at daily doses of about 50 mg have claimed an increase in mental acuity. There are no reports available of adverse effects from consumption of excess thiamine by ingestion of food and supplements. Because the data are inadequate for a quantitative risk assessment, no Tolerable Upper Intake Level (UL) can be derived for thiamine.
Antagonists
Thiamine in foods can be degraded in a variety of ways. Sulfites, which are added to foods usually as a preservative, will attack thiamine at the methylene bridge in the structure, cleaving the pyrimidine ring from the thiazole ring. The rate of this reaction is increased under acidic conditions. Thiamine is degraded by thermolabile thiaminases (present in raw fish and shellfish). Some thiaminases are produced by bacteria. Bacterial thiaminases are cell surface enzymes that must dissociate from the membrane before being activated; the dissociation can occur in ruminants under acidotic conditions. Rumen bacteria also reduce sulfate to sulfite, therefore high dietary intakes of sulfate can have thiamine-antagonistic activities.
Plant thiamine antagonists are heat stable and occur as both the ortho and para hydroxyphenols. Some examples of these antagonists are caffeic acid, chlorogenic acid and tannic acid. These compounds interact with the thiamine to oxidize the thiazole ring, thus rendering it unable to be absorbed. Two flavonoids, quercetin and rutin, have also been implicated as thiamine antagonists.
Absorption and transport
Absorption
Thiamine is released by the action of phosphatase and pyrophosphatase in the upper small intestine. At low concentrations the process is carrier mediated and at higher concentrations, absorption occurs via passive diffusion. Active transport is greatest in the jejunum and ileum (it is inhibited by alcohol consumption and by folic deficiency. Decline in thiamine absorption occurs at intakes above 5 mg. The cells of the intestinal mucosa have thiamine pyrophosphokinase activity, but it is unclear whether the enzyme is linked to active absorption. The majority of thiamine present in the intestine is in the pyrophosphorylated form ThDP, but when thiamine arrives on the serosal side of the intestine it is often in the free form. The uptake of thiamine by the mucosal cell is likely coupled in some way to its phosphorylation/dephosphorylation. On the serosal side of the intestine, evidence has shown that discharge of the vitamin by those cells is dependent on Na+-dependent ATPase.
Bound to serum proteins
The majority of thiamine in serum is bound to proteins, mainly albumin. Approximately 90% of total thiamine in blood is in erythrocytes. A specific binding protein called thiamine-binding protein (TBP) has been identified in rat serum and is believed to be a hormonally regulated carrier protein that is important for tissue distribution of thiamine.
Cellular uptake
Uptake of thiamine by cells of the blood and other tissues occurs via active transport and passive diffusion.+ and a transcellular proton gradient. About 80% of intracellular thiamine is phosphorylated and most is bound to proteins. In some tissues, thiamine uptake and secretion appears to be mediated by a soluble thiamine transporter that is dependent on Na
Tissue distribution
Human storage of thiamine is about 25 to 30 mg with the greatest concentrations in skeletal muscle, heart, brain, liver, and kidneys. ThMP and free (unphosphorylated) thiamine is present in plasma, milk, cerebrospinal fluid, and likely all extracellular fluids. Unlike the highly phosphorylated forms of thiamine, ThMP and free thiamine are capable of crossing cell membranes. Thiamine contents in human tissues are less than those of other species.
Excretion
Thiamine and its acid metabolites (2-methyl-4-amino-5-pyrimidine carboxylic acid, 4-methyl-thiazole-5-acetic acid and thiamine acetic acid) are excreted principally in the urine.
Thiamine phosphate derivatives and function
Thiamine is mainly the transport form of the vitamin, while the active forms are phosphorylated thiamine derivatives. There are four known natural thiamine phosphate derivatives: thiamine monophosphate (ThMP), thiamine diphosphate (ThDP), also sometimes called thiamine pyrophosphate (TPP), thiamine triphosphateadenosine thiamine triphosphate (AThTP) and adenosine thiamine diphosphate (AThDP). (ThTP), and the recently discovered
Thiamine monophosphate
There is no known physiological role of ThMP.
Thiamine diphosphate
The synthesis of thiamine diphosphate (ThDP), also known as thiamine pyrophosphate (TPP) or cocarboxylase, is catalyzed by an enzyme called thiamine diphosphokinase according to the reaction thiamine + ATP → ThDP + AMP (EC 2.7.6.2). ThDP is a coenzyme for several enzymes that catalyze the transfer of two-carbon units and in particular the dehydrogenation (decarboxylation and subsequent conjugation with coenzyme A) of 2-oxoacids (alpha-keto acids). Examples include:
- Present in most species
- pyruvate dehydrogenase and 2-oxoglutarate dehydrogenase (also called α-ketoglutarate dehydrogenase)
- branched-chain α-keto acid dehydrogenase
- 2-hydroxyphytanoyl-CoA lyase
- transketolase
- Present in some species:
- pyruvate decarboxylase (in yeast)
- several additional bacterial enzymes
The enzymes transketolase, pyruvate dehydrogenase (PDH) and 2-oxoglutarate dehydrogenase (OGDH) are all important in carbohydrate metabolism. The cytosolic enzyme transketolase is a key player in the pentose phosphate pathway, a major route for the biosynthesis of the pentose sugars deoxyribose and ribose. The mitochondrial PDH and OGDH are part of biochemical pathways that result in the generation of adenosine triphosphate (ATP), which is a major form of energy for the cell. PDH links glycolysis to the citric acid cycle, while the reaction catalyzed by OGDH is a rate-limting step in the citric acid cycle. In the nervous system, PDH is also involved in the production of acetylcholine, a neurotransmitter, and for myelin synthesis.
Thiamine triphosphate
Thiamine triphosphate (ThTP) was long considered a specific neuroactive form of thiamine. However, recently it was shown that ThTP exists in bacteria, fungi, plants and animals suggesting a much more general cellular role.In particular in E. coli, it seems to play a role in response to amino acid starvation.
Adenosine thiamine triphosphate
Adenosine thiamine triphosphate (AThTP) or thiaminylated adenosine triphosphate has recently been discovered in Escherichia coli where it accumulates as a result of carbon starvation. In E. coli, AThTP may account for up to 20 % of total thiamine. It also exists in lesser amounts in yeast, roots of higher plants and animal tissue.
Adenosine thiamine diphosphate
Adenosine thiamine diphosphate (AThDP) or thiaminylated adenosine diphosphate exists in small amounts in vertebrate liver, but its role remains unknown.
Deficiency
Thiamine derivatives and thiamine-dependent enzymes are present in all cells of the body, thus, a thiamine deficiency would seem to adversely affect all of the organ systems. However, the nervous system and the heart are particularly sensitive to thiamine deficiency, because of their high oxidative metabolism.
Thiamine deficiency can lead to severe fatigue of eyes and myriad problems including neurodegeneration, wasting and death. A lack of thiamine can be caused by malnutrition, a diet high in thiaminase-rich foods (raw freshwater fish, raw shellfish, ferns) and/or foods high in anti-thiamine factors (tea, coffee, betel nuts) and by grossly impaired nutritional status associated with chronic diseases, such as alcoholism, gastrointestinal diseases, HIV-AIDS, and persistent vomiting. It is thought that many people with diabetes have a deficiency of thiamine and that this may be linked to some of the complications that can occur.
Well-known syndromes caused by thiamine deficiency include beriberi and Wernicke-Korsakoff syndrome, diseases also common with chronic alcoholism.
Beriberi
Beriberi is a neurological and cardiovascular disease. The three major forms of the disorder are dry beriberi, wet beriberi, and infantile beriberi
- Dry beriberi is characterized principally by peripheral neuropathy consisting of symmetric impairment of sensory, motor, and reflex functions affecting distal more than proximal limb segments and causing calf muscle tenderness.
- Wet beriberi is associated with mental confusion, muscular wasting, edema, tachycardia, cardiomegaly, and congestive heart failure in addition to peripheral neuropathy.
- Infantile beriberi occurs in infants breast-fed by thiamin-deficient mothers (who may show no sign of thiamine deficiency). Infants may manifest cardiac, aphonic, or pseudomeningitic forms of the disorder. Infants with cardiac beriberi frequently exhibit a loud piercing cry, vomiting, and tachycardia.Convulsions are not uncommon, and death may ensue if thiamine is not administered promptly.
Following thiamine treatment, rapid improvement occurs generally within 24 hours. Improvements of peripheral neuropathy may require several months of thiamine treatment.
Alcoholic brain disease
Nerve cells and other supporting cells (such as glial cells) of the nervous system require thiamine. Examples of neurologic disorders that are linked to alcohol abuse include Wernicke’s encephalopathy (WE, Wernicke-Korsakoff syndrome) and Korsakoff’s psychosis (alcohol amnestic disorder) as well as varying degrees of cognitive impairment.
Wernicke’s encephalopathy is the most frequently encountered manifestation of thiamine deficiency in Western society, though it may also occur in patients with impaired nutrition from other causes, such as gastrointestinal disease, those with HIV-AIDS, and with the injudicious administration of parenteral glucose or hyperalimentation without adequate B-vitamin supplementation. This is a striking neuro-psychiatric disorder characterized by paralysis of eye movements, abnormal stance and gait, and markedly deranged mental function.
Alcoholics may have thiamine deficiency because of the following:
- inadequate nutritional intake: alcoholics tend to intake less than the recommended amount of thiamine.
- decreased uptake of thiamine from the GI tract: active transport of thiamine into enterocytes is disturbed during acute alcohol exposure.
- liver thiamine stores are reduced due to hepatic steatosis or fibrosis.
- impaired thiamine utilization: magnesium, which is required for the binding of thiamine to thiamine-using enzymes within the cell, is also deficient due to chronic alcohol consumption. The inefficient utilization of any thiamine that does reach the cells will further exacerbate the thiamine deficiency.
- Ethanol per se inhibits thiamine transport in the gastrointestinal system and blocks phosphorylation of thiamine to its cofactor form (ThDP).
Korsakoff Psychosis is generally considered to occur with deterioration of brain function in patients initially diagnosed with WE.. This is an amnestic-confabulatory syndrome characterized by retrograde and anterograde amnesia, impairment of conceptual functions, and decreased spontaneity and initiative.<
Following improved nutrition and the removal of alcohol consumption, some impairments linked with thiamine deficiency are reversed; particularly poor brain functionality, although in more severe cases, Wernicke-Korsakoff syndrome leaves permanent damage. (See delirium tremens.)
Thiamine deficiency in poultry
As most feedstuffs used in poultry diets contain enough quantities of vitamins to meet the requirements in this species, deficiencies in this vitamin does not occur with commercial diets. This was, at least, the opinion in the 1960s.
Mature chickens show signs 3 weeks after being fed a deficient diet. In young chicks, it can appear before 2 weeks of age.
Onset is sudden in young chicks. There is anorexia and an unsteady gait. Later on, there are locomotor signs, beginning with an apparent paralysis of the flexor of the toes. The characteristic position is called "stargazing", meaning a chick "sitting on its hocks and the head in opisthotonos.
Response to administration of the vitamin is rather quick, occurring a few hours later.
Differential diagnosis include riboflavin deficiency and avian encephalomyelitis. In riboflavin deficiency, the "curled toes" is a characteristic symptom. Muscle tremor is typical of avian encephalomyelitis. A therapeutic diagnosis can be tried by supplementing Vitamin B1 only in the affected bird. If the animals do not respond in a few hours, Vitamin B1 deficiency can be excluded.
Thiamine deficiency in ruminants
Polioencephalomalacia(PEM), is the most common thiamine deficiency disorder in young ruminant and nonruminant animals. Symptoms of PEM include a profuse, but transient diarrhea, listlessness, circling movements, star gazing or opisthotonus (head drawn back over neck), and muscle tremors. The most common cause is high-carbohydrate feeds, leading to the overgrowth of thiaminase-producing bacteria, but dietary ingestion of thiaminase (e.g. in bracken fern), or inhibition of thiamine absorption by high sulfur intake are also possible.
Idiopathic paralytic disease in wild birds
Recently thiamine deficiency has been identified as the cause of a paralytic disease affecting wild birds in the Baltic Sea area dating back to 1982. In this condition, there is difficulty in keeping the wings folded along the side of the body when resting, loss of the ability to fly and voice with eventual paralysis of the wings and legs and death. It affects primarily 0.5–1 kg sized birds such as the herring gull (Larus argentatus), Common Starling (Sturnus vulgaris) and Common Eider (Somateria mollissima). Researches noted "Because the investigated species occupy a wide range of ecological niches and positions in the food web, we are open to the possibility that other animal classes may suffer from thiamine deficiency as well."p. 12006
Analysis and diagnostic testing
A positive diagnosis test for thiamine deficiency can be ascertained by measuring the activity of the enzyme transketolase in erythrocytes (Erythrocyte Transketolase Activation Assay). Thiamine, as well as its phosphate derivatives, can also be detected directly in whole blood, tissues, foods, animal feed and pharmaceutical preparations following the conversion of thiamine to fluorescent thiochrome derivatives (Thiochrome Assay) and separation by high performance liquid chromatography (HPLC).In recent reports, a number of Capillary Electrophoresis (CE) techniques and in-capillary enzyme reaction methods have emerged as potential alternative techniques for the determination and monitoring of thiamine in samples.
Genetic diseases
Genetic diseases of thiamine transport are rare but serious. Thiamine Responsive Megaloblastic Anemia is an autosomal recessive disorder caused by mutations in the gene SLC19A2, a high affinity thiamine transporter. TRMA patients do not show signs of systemic thiamine deficiency, suggesting redundancy in the thiamine transport system. This has led to the discovery of a second high affinity thiamine transporter, SLC19A3. Leigh Disease (Subacute Necrotising Encephalomyelopathy) is an inherited disorder which affects mostly infants in the first years of life and is invariably fatal. Pathological similarities between Leigh disease and WE led to the hypothesis that the cause was a defect in thiamine metabolism. One of the most consistent findings has been an abnormality of the activation of the pyruvate dehydrogenase complex with diabetes mellitus and sensorineural deafness (TRMA)
Other disorders in which a putative role for thiamine has been implicated include Subacute Necrotizing Encephalomyelopathy, Opsoclonic Cerebellopathy (a paraneoplastic syndrome), and Nigerian Seasonal Ataxia. In addition, several inherited disorders of ThDP-dependent enzymes have been reported, which may respond to thiamine treatment.
Label: Pharmacy
0 Comments:
Subscribe to:
Posting Komentar (Atom)








